Diseases And Disorders Of The Retina, Types, Causes And Treatment
Once the images are captured by a series of specialized cells, called photoreceptors, they are sent through the nerve fibres to the optic nerve, which contains approximately one million of them, and finally to the areas of the brain that manage vision.
Due to its characteristics, the retina can be considered part of the brain, and for this reason, it participates in a whole series of neurological pathologies of all kinds: congenital, degenerative, metabolic, etc.
God Service Eye Clinic will focus on perhaps the most common pathologies that affect the retina, although there are some that are exclusive to certain age groups, such as retinoblastoma.
Retinal detachment
The most common type is the one produced by the appearance of a tear in the peripheral retina, through which fluid can penetrate and detach a retinal bag, which can progress to affect the area richest in photoreceptors, called the macula, or even produce the detachment of the entire retina.
The origin of these tears can be of a traumatic type, due to traction in the “collapse” of the vitreous humour, (frequent from the age of 50 with the appearance of the so-called “floaters”) or from debilitating degenerations of the retina. , generally in myopes of more than three diopters.
The retinal detachment may or may not be preceded by the display of flashes and/or “floaters”, finally appearing in an area without vision (vision in the curtain) that may become larger.
Treatment is a relative urgency and generally consists of plugging the causative tear, draining the fluid, and a series of methods aimed at applying the detached retina to the underlying layers.
If sudden flashes or floaters appear, it is important to go to the ophthalmologist, because if the tear is detected before the detachment occurs, it can be “welded” with a laser and avoided. In high myopic patients, periodic review of the peripheral retina is also very important, even if they are asymptomatic.
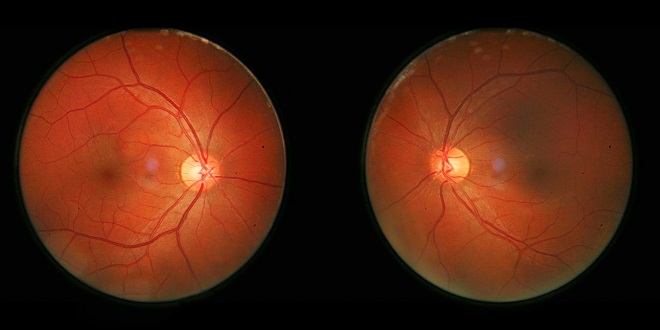
Diabetic retinopathy
In the evolution of Diabetes, both type 1 and 2, a series of changes occur in the vessels of the body. This deterioration, in the retinal vessels, can cause serious damage to visual function if an early diagnosis is not made and adequate treatment is instituted.
diagram on retinopathyThe so-called Diabetic Retinopathy, usually starts, depending on the metabolic control of the patient, approximately 10 years after the onset of the disease, and consists of the loss of cells (Pericytes) that stabilize the structure of the capillaries.
Thus, initially phenomena of “herniation” occur in the capillaries called microaneurysms, as well as an increase in their permeability with an accumulation of cholesterol salts with a shiny, yellowish-white appearance (hard exudates).
The rupture of microaneurysms can also produce a series of microhemorrhages of various shapes and sizes. This stage is called Background Diabetic Retinopathy.
In the evolution of the disease, capillary occlusion phenomena occur, true microinfarcts, which are represented by the appearance on the retina of whitish spots less bright than those previously described, called soft exudates. This stage is called Pre-Proliferative Diabetic Retinopathy.
These microinfarcts herald greater complications, since they produce areas of non-perfusion in the retina, which stimulate the formation of humoral factors such as VEGF, which tries to stimulate the formation of new vessels (neovessels) that provide blood flow to the ischemic areas.
This attempt, far from improving the situation, makes it worse, since these new vessels are fragile and bleed profusely easily, or they retract and fibrosis, producing haemorrhages, which can fill the posterior cavity of the eye with blood and prevent vision for months, and even detach the retina due to the retraction. This phase is called Proliferative Diabetic Retinopathy, due to the proliferation of these neovessels.
Regarding the diagnosis of diabetic retinopathy, early diagnosis is of vital importance, therefore an annual assessment of the fundus is recommended to detect initial lesions.
If lesions already appear, a test called Angiofluoresceingraphy is useful, which consists of observing the behaviour of contrast injected into a vein and taking a series of aerial photographs, which will indicate areas of leakage or areas of poorly perfused retina ( ischemic).
The treatment consists, initially, of the application of a laser that will heal the leaking points (microaneurysm) and/or will eliminate the ischemic areas that we will sacrifice to avoid the secretion of vascular proliferative factors and the appearance of the devastating neovessels.
There are also complex surgical techniques to treat major complications such as vitreous haemorrhages and tractional retinal detachments. (vitrectomy).
Macular degeneration
Associated with Age (ARMD): In a significant percentage of the population over 60 years of age, degenerative changes are observed in the central area of the retina. This area called the Macula, (“spot”, due to the accumulation of yellowish pigments) is responsible for 90% of the vision we use (central), as well as colour vision, due to the presence of “cones”, photoreceptors specialized in colour vision.
The origin of AMD is usually multifactorial, in addition to age, factors such as a diet low in carotenes and antioxidants, tobacco, sun exposure, etc.
The lesions that can be seen are basically of two types: Areas of atrophy that characterize the most frequent type of AMD, called “Dry AMD”. There is a progressive and slow loss of central vision. This type of degeneration currently has no treatment, although the progress can be slowed down with antioxidant supplements.
Another type of AMD is the so-called Wet, which consists of the formation of whitish and globular lesions composed of “waste” materials from the retina, called “Drusen”.
These lesions end up producing, on occasion, a break in a layer of the retina, which stimulates the formation of new vessel membranes that ascend from the lower layers (choroid) towards the retina.
As in diabetic retinopathy, these new vessels can exude or even bleed, causing a sudden decrease in visual acuity, with the presence of deformations of objects (metamorphopsia) that reproduce the “bulges” of the edematous retina or black spots in the visual field called scotomas.
Regarding diagnosis, we also use Angiofluoresceingraphy and, for some years now, the so-called Optical Coherence Tomography, which offers us images of retinal sections similar to a scanner.
The treatment consists of repeated injection inside the eyeball of substances that inhibit VEGF, causing, as in diabetes, neovascular formations.